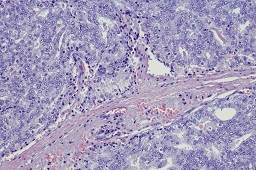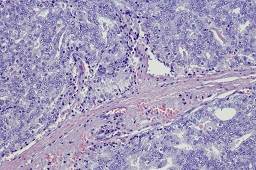
The MSI-H/dMMR phenotype is uncommon among men with advanced prostate cancer, but its presence is associated with greater likelihood of a durable response to PD-1/PD-L1 inhibitors.
Immune checkpoint blockade may benefit men with advanced prostate cancer (PCa) who have an uncommon molecular phenotype, a new study suggests.
The phenotype—microsatellite instability-high (MSI-H) or mismatch repair-deficient (dMMR) PCa—may be somatically acquired during disease evolution and its presence appears to indicate a greater likelihood of a durable response to inhibitors of programmed cell death protein 1 (PD-1)/programmed cell death 1 ligand 1 (PD-L1), according to investigators. This potential for durable response to these medications supports prospective tumor sequencing to screen all men with advanced PCa for MSI-H/dMMR, according to a research team led by Wassim Abida, MD, PhD, of Memorial Sloan Kettering Cancer Center in New York.
Dr Abida and his collaborators examined the prevalence of this phenotype and its association with response to immune checkpoint blockade in 1346 patients with PCa. All had undergone paired tumor and germline sequencing. Of 1033 patients who had adequate tumor quality for MSIsensor analysis, 32 (3.1%) had MSI-H/dMMR disease and 23 (2.2%) had tumors with high MSIsensor scores, the investigators reported in JAMA Oncology.1 Among the 32 patients with MSI-H/dMMR tumors, 7 (21.9%) carried a germline mutation in a Lynch syndrome–associated gene.
In addition, 11 patients with MSI-H/dMMR castration-resistant PCa received anti–PD-1/PD-L1 therapy, with 6 (54.5%) experiencing a greater than 50% decline in PSA (4 of whom had radiographic responses). As of May 2018, 5 of the 11 patients remained on therapy for up to 89 weeks.
An important step
Commenting on the new study, Soroush Rais-Bahrami, MD, an associate professor at the University of Alabama (UAB) in Birmingham, director of the UAB Program for Personalized Prostate Care, and researcher at UAB’s O’Neal Comprehensive Cancer Center, said the findings are an important step in better defining what percentage of patients with aggressive PCa may benefit from PD1/PD-L1 inhibitor therapy. This also helps advance the field of precision medicine for men with aggressive PCa. “It is very commendable work, and it is going to help improve our understanding of how these [immune checkpoint inhibitor] agents are going to be used as we move forward,” Dr Rais-Bahrami told Renal & Urology News.
Manish Kohli, MD, Vice-Chair, Department of Genitourinary Oncology and Director of the DeBartolo Family Personalized Medicine Institute at Moffitt Cancer Center in Tampa, Florida, these findings show that 3.1% of all patients with PCa harbor dMMR/MSI-H genomic profiles, which is in line with a previously published study that looked at 12,019 different tumors and the percentage of mismatch repair deficient (d-MMR) tumors in each cancer subtype.2 “This study confirms the same figure. However, this study also adds the finding that, in patients who harbor these type of genomic abnormalities, what would be the outcome if those patients were to be treated with immunotherapy,” Dr Kohli said.
Screening questioned
According to Dr Kohli, the low prevalence raises a question: Is worth testing all men with advanced PCa when only up to 3 cases would be detected for every 100 men tested for this type of abnormality and only half of those will actually benefit from the treatment? “As this is the stage where immunotherapies are given in prostate cancer,” Dr Kohli said, “it becomes important to know the individual patient with type of abnormality since the clinical impact is that we will need to offer testing to nearly 100 advanced prostate cancer patients to identify perhaps 1 to 2 patients in advanced stages who have such abnormalities. While this is absolutely important for those 2 patients to successfully get treated and in fact is the reason for personalizing expensive and toxic cancer treatments, the recognition is that it comes at a cost of testing quite a few more patients.”
Zachary Hamilton, MD, assistant professor of urology at Saint Louis University School of Medicine, St. Louis, Missouri, said the authors of the new study should be applauded for their investigation. The findings highlight the growing possibilities with genetically targeted therapy and patient-tumor specific treatment recommendations in the management of prostate cancer. “Although the absolute number of patients with high MSI sensor scores was low, it appears that many of them had strong responses to anti-PD-1/PD-L1 therapy, Dr Hamilton said. “These findings are both surprising but encouraging for those individual patients.”
Later targeted therapy?
He said the idea of personalized medicine is an important topic in treating all tumor types. He said other studies have investigated various aspects of PCa genetics, such as AR-V7. “There may be a time in the future when patients can receive genetically targeted treatments from the day of initial diagnosis,” he said. “However, current studies such as this provide the ability to consider targeted therapy later in the treatment course and will certainly shape guideline statements.”
References
1. Abida W, Cheng ML, Armenia J, et al. Analysis of the prevalence of microsatellite instability in prostate cancer and response to immune checkpoint blockade. JAMA Oncol. 2018; published online ahead of print.
2. Le DT, Durham JN, Smith KN et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science. 2017;357(6349):409-413.